Science: How Heat Reduces Male Fertility

KEY POINTS
- sperm counts are down 50% over the last 40 years
- healthy sperm are extremely sensitive to testicular overheating
- daily overheating by just 2 deg. from body heat (sitting) causes sperm count and sperm motility to plummet by over 90%
- overheating can be caused by sitting or driving for longer than 20 minutes, obesity, varicocele, and hot environments
- overheating may cause permanent, abnormal changes to DNA gene expression in offspring via epigenetic pathways, leading to disease or other complications
- on average, men now sit for >12 hours per day
- The Underdog prevents testicular overheating when sitting
Why Sperm Count Matters
Scientific research establishes that a higher sperm count correlates with increased fertility. As sperm counts in men rise from zero to 40 million/ml, there is a progressive increase in the chances of their partner becoming pregnant [1].
For example, in a study of 430 couples trying to conceive over a 6-month study period, the conception rate was 36% for men with less than 20 million/ml, and 65% for men with greater than 20 million/ml [2].
And evidence suggests [3] that better sperm morphology (a measure of quality) leads to improved fertility.
Sperm Counts in Decline
Researchers have recently confirmed an alarming trend: western male sperm count has dropped by 50-60% over the last 40 years with no signs of leveling-off. This is detailed in a recent 2017 meta-study [4] by Levine et al that caught the attention of world media, where researchers analyzed 183 sperm count data sets collected over the last 40 years from men in America, Europe, Australia and New Zealand.

Fig. 1: Western Sperm Count Down 50% [4]
While the root causes are still under investigation, overheating remains a prime suspect. During the same 40 year span our modern lifestyles have changed to more sedentary office jobs, increased commuting time, and increased screen time - all of which involve more sitting (and therefore scrotal heating) than ever before [5]. And our steady rise in body fat percentage over this same period [6] is another factor adding to scrotal heating and reduced sperm count [7].
Heat Kills Sperm
The testicular tissues are exquisitely sensitive to even mild overheating. Numerous studies have shown that a small temperature rise in human scrotal temperature leads to dramatic depression of total sperm count and sperm motility, and a degradation in the quality (morphology) of the remaining sperm.
Robinson & Rock [8] exposed a group of 10 healthy men to a 0.8 deg. C scrotal temperature rise for 15 hours per day. This lead to an 80% reduction in sperm count in the 2-3 month time period following such exposure.
Mieusset et al [9, 10] exposed a group of 14 healthy men with normal 34 deg. C scrotums to a 2 deg. C temperature rise for 15 hours per day using their own body heat. This lead to a 90% reduction in sperm count and sperm motility, and a 35% reduction in normal sperm morphology of the few sperm that remained. These effects all but disappeared 3-4 months after stopping the temperature rise.
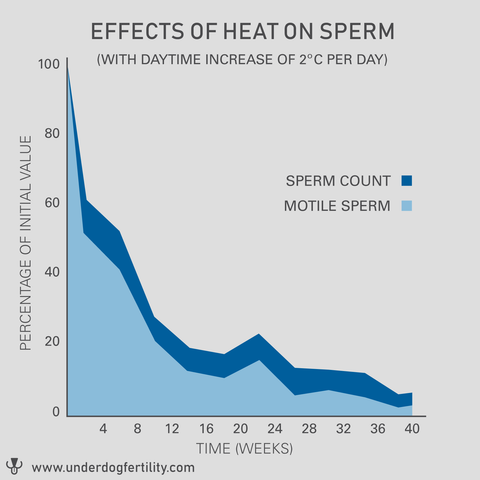
Fig. 2: Detrimental Effects of 2 deg. C Rise on Sperm Count, Motility, and Morphology [9,10]
Hjollund et al [11] took temperature measurements and sperm samples among 101 test subjects, and found a negative correlation whereby sperm concentration decreased 40% per 1 deg. C. increment of median daytime scrotal temperature.
Another study by Hjollund [12] measured median sperm concentration in a group of 66 men. Men with higher scrotal temperatures (above 35 deg. C for more than 75% of daytime) had at the median a 64% lower sperm concentration than men with lower scrotal temperatures (below 35 deg. C for at least 50% of the day).
Sitting and Driving Cause Overheating
Sitting defeats the scrotum’s natural cooling mechanisms that rely on exposed surface area. This makes the testicle temperature rapidly rise to where normal sperm formation cannot occur.
Jung et al [13] tested a group of 8 healthy men in various postures. During 1 hour phases of sitting at a writing desk or in a car, temperatures increased 2 deg. C to around the dangerous 36 deg. C mark. In contrast, values were in a safer region below 35 deg. C during a walking phase.
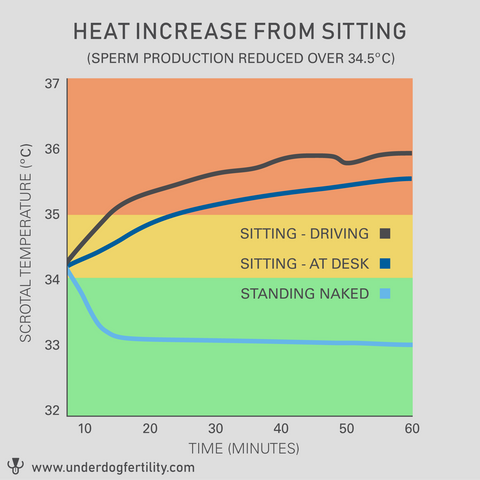
Fig. 3: Scrotal Heating from Sitting and Driving vs Walking [13]
Jung et al [14] tested a larger group of 50 healthy men in sitting vs walking posture. After 20 minutes of sitting, subjects experienced an average 2 deg. C scrotal temperature rise.
Bengoudifa & Mieusset [15] measured a group of 8 fertile volunteers and established that wearing clothing in a seated position was responsible for a 1.5 to 2 deg. C temperature rise as compared to a more natural standing position.
Bujan et al [16] found in a group of 9 healthy men that walking clothed outdoors resulted in a healthy mean 34.2 deg. C scrotal temperature, but driving a car caused a spike in scrotal temperature by 1.7 to 2.2 deg. C.

Fig. 4: Scrotal Heating from Driving [16]
Heat from Varicocele and Obesity
A BMI greater than 25 is associated with an average 25% reduction in sperm count and sperm motility [19]. Higher levels of fatty tissue in the inner thigh and scrotal region cause higher testicular temperatures by inhibiting scrotal cooling mechanisms. [20] [21] [22] [23].
Varicocele is a condition of varicose veins in the scrotum. It affects 15% of the male population (including an Underdog founder!), and has a high correlation with male infertility - up to 35% of males with infertility have varicocele [7]. Scrotal overheating from increased blood-flow is the most likely mechanism whereby Varicocele reduces male fertility [7].
Garolla et al [7] monitored scrotal temperatures over a period of 2 years in a group of 80 men, 60 of which had risk factors for testicular heating such as varicocele or obesity. It was found that men with either varicocele or obesity showed higher scrotal temperatures, and these higher temperatures were related to a significant negative alteration of spermatogenesis.
Heat-Stress Induced DNA and Epigenetic Changes in Children
Inheritance of DNA-determined traits is not as simple as once thought. Epigenetic mechanisms involve DNA and histone modifications and result in the heritable silencing of genes without a change in their coding sequence. Disruption of the balance of epigenetic networks may cause major pathologies.
New research into paternal factors [24] [25] [26] [27] [20] suggest that environmental factors such as heat stress on the father's body impact the offspring's inherited traits via epigenetic mechanisms, potentially causing lasting negative outcomes in offspring.
To reduce the chances of this, it is important to ensure sperm formation is optimized through reduction of stressors on the father's sperm such as testicular overheating.
What Can We Conclude?
- Optimal sperm formation occurs a full 3 degrees Celsius (5.4 deg. F) below body temperature.
- Healthy sperm formation is extremely sensitive to heat.
- A 1 deg. C rise in scrotal temperature reduces count by 40%
- A 2 deg. C rise reduces sperm count and motility to nearly zero, and significantly impacts morphology.
- Heat stressed sperm produce changes in DNA and gene expression in offspring
- Risk factors for overheating include sitting, driving, obesity, varicocele, and hot environments.
Enter The Underdog

In a small study, The Underdog was shown to reduce the rise in scrotal temperature by 2 to 3 deg. C when clothed and seated, to keep the scrotum mean temperature in the optimal 33-34 deg. C range where sperm formation is optimized.
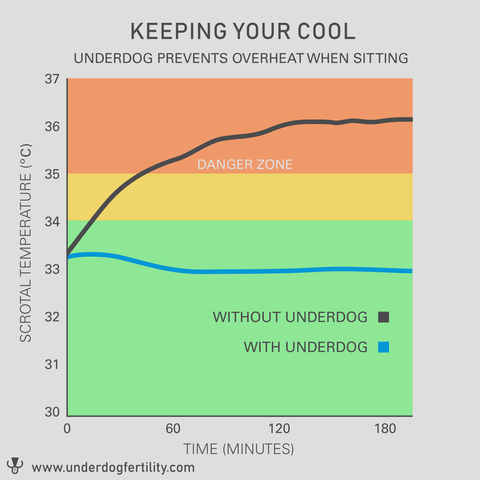
And most importantly, The Underdog is engineered to be safe. The non-invasive design presents no risk or discomfort to the genitals. And the level of cooling is very gentle, well-controlled, and consistent, unlike a competitor’s underwear-based solution that provides a too-extreme level of cooling.
The Underdog helps sperm reach their true potential using its patented safe, gentle method of cooling.
References
[1] Sharpe, 2012. Sperm counts and fertility in men: a rocky road ahead. EMBO Reports, 2012 May; 13(5): 398–403.
[2] Bonde et al, 1998. Relation between semen quality and fertility: a population-based study of 430 first-pregnancy planners. The Lancet, 1998 Oct 10;352(9135):1172-7.
[3] Menkveld et al, 2011. Measurement and significance of sperm morphology. Asian Journal of Andrology, 2011 Jan; 13(1): 59–68.
[4] Levine et al, 2017. Temporal trends in sperm count: a systematic review and meta-regression analysis. Human Reproduction Update, Volume 23, Issue 6, 1 November 2017, Pages 646–659.
[5] Owen et al, 2010. Sedentary Behavior: Emerging Evidence for a New Health Risk. Mayo Clinic Proceedings, 2010 Dec; 85(12): 1138–1141.
[6] Pribis et al, 2010. Trends in Body Fat, Body Mass Index and Physical Fitness
Among Male and Female College Students. Journal of Nutrients 2010, 2, 1075-1085; doi:10.3390/nu2101075.
[7] Garolla et al, 2015. Twenty-four-hour monitoring of scrotal temperature in obese men and men with a varicocele as a mirror of spermatogenic function. Journal of Human Reproduction, Volume 30, Issue 5, 1 May 2015, Pages 1006–1013.
[8] Robinson & Rock, 1967. Intrascrotal hyperthermia induced by scrotal insulation: effect on spermatogenesis. Journal of Obstetrics and Gynecology, 1967 Feb;29(2):217-23.
[9] Mieusset et al, 1985. Inhibiting effect of artificial cryptorchidism on spermatogenesis. Journal of Fertility and Sterility, 1985 Apr;43(4):589-94.
[10] Mieusset et al, 1987. Association of scrotal hyperthermia with impaired spermatogenesis in infertile men. Journal of Fertility and Sterility, 1987 Dec;48(6):1006-11.
[11] Hjollund et al, 2002. The relation between daily activities and scrotal temperature. Reproductive Toxicology, May 2002, 16(3):209-214.
[12] Hjollund et al, 2000. Diurnal scrotal skin temperature and semen quality. International Journal of Andrology Vol. 23, Issue 5, Oct 2000. pp 309-318.
[13] Jung et al, 2001. Genital heat stress as a threat to male fertility. Andrologia, 33, 316-317.
[14] Jung et al, 2005. Influence of the type of undertrousers and physical activity on scrotal temperature. Journal of Human Reproduction Vol.20, No.4 pp. 1022–1027, 2005.
[15] Bengoudifa & Mieusset, 2007. Effect of posture and clothing on scrotal temperature in fertile men. Journal of Andrology 2007 Jan-Feb;28(1):170-5. Epub 2006 Sep 6.
[16] Bujan et al, 2000. Increase in scrotal temperature in car drivers. Journal of Human Reproduction vol. 15 no. 6 pp 1355-1357, 2000.
[17] Bonde, 1992. Semen quality in welders exposed to radiant heat. British Journal Independent Medicine, 1992, Jan., vol 49, pp 5-10.
[18] Thonneau et al, 1998. Occupational heat exposure and male fertility: a review. Journal of Human Reproduction, Volume 13, Issue 8, 1 August 1998, Pages 2122–2125.
[19] Hammoud et al, 2008. Impact of male obesity on infertility: a critical review of the current literature. Journal of Fertility and Sterility, 2008 Oct;90(4):897-904.
[20] Liu & Ding, 2017. Obesity, a serious etiologic factor for male subfertility in modern society. Journal of Reproduction, 2017 Oct;154(4):R123-R131.
[21] Kahn & Brannigan, 2017. Obesity and male infertility. Current Opinion in Urology, 2017 Sep;27(5):441-445.
[22] Katib, 2015. Mechanisms linking obesity to male infertility. Central European Journal of Urology, 2015; 68(1): 79–85.
[23] Phillips and Tanphaichitr, 2010. Mechanisms of obesity-induced male infertility. Expert review Endocrinology & Metabolism. March 2010. 5(2):229-251.
[24] Rahman et al, 2018 Heat stress responses in spermatozoa: Mechanisms and consequences for cattle fertility. Theriogenology, June 2018.
[25] Gannon et al, 2014 The Sperm Epigenome: Implications for the Embryo. Advances in Experimental Medicine and Biology, January 2014.
[26] Jenkins and Carrell, 2012. The sperm epigenome and potential implications for the developing embryo. Journal of Reproduction, Jun 2012.
[27] Braun et al, 2017. Fathers Matter: Why It's Time to Consider the Impact of Paternal Environmental Exposures on Children's Health. Current Epidemiological Reports. March 2017.
